On its surface, the mental health reform bill introduced by Congressman Tim Murphy looks promising. On closer inspection, however, the “Murphy Bill” appears to serve the pharmaceutical companies more than the people.
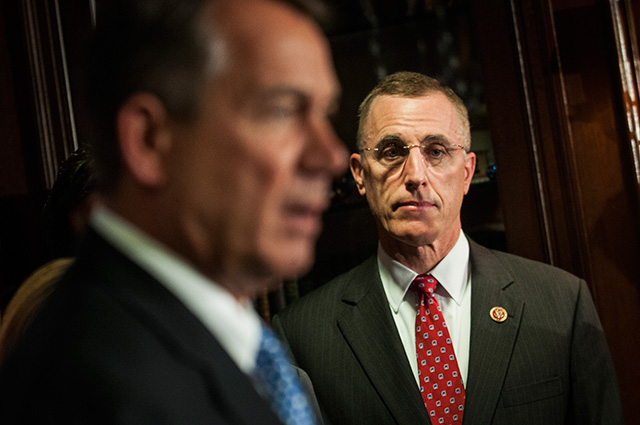
Rep. Tim Murphy (R-Pennsylvania), right, and former House Speaker John Boehner (R-Ohio) during a news conference about the Affordable Care Act at the Republican National Committee headquarters in Washington, October 23, 2013. (Gabriella Demczuk / The New York Times)
On its surface, the mental health reform bill introduced by Congressman Tim Murphy of Pennsylvania looks promising. Murphy is the only licensed psychologist in Congress, everybody agrees that our mental health system is not working, and we would all like
to help families in crisis.
On closer inspection, however, the Helping Families in Mental Health Crisis Act (HR 2646) – commonly known as the “Murphy Bill” – appears to cater more closely to
the desires of pharmaceutical companies than to the actual needs of people in psychological distress, perhaps because of Murphy’s connections to key lobbyists.
Murphy’s financial supporters include the American Psychiatric Association, psychiatric hospitals and the National Rifle Association, and his campaign contributors include
no less than nine pharmaceutical companies and a law firm that represents Big Pharma.
The bill was marked up Wednesday in the House Energy and Commerce health subcommittee and passed by that subcommittee, despite strong objections from almost all the Democrats on the full committee.
The next step is for the full Energy and Commerce Committee to vote on moving the bill forward, followed by the House vote. A timetable has not yet been set. Although the bill is gaining momentum, there is substantial opposition, so passage is still
uncertain.
If the Murphy Bill is passed, psychiatric hospitals and pharmaceutical companies will reap huge financial benefits as a result of increased hospitalization and forced treatment. One way the bill will do this is by creating a financial incentive for states
that implement “assisted outpatient treatment”: court-ordered treatment (including medication) for people whom a judge deems as living with “severe mental illness” and unlikely to willingly take prescribed psychiatric medications.
Psychiatric hospitals would also benefit from the bill’s proposed elimination of the “Institutions for Mental Diseases exclusion,” which currently makes mental health institutions ineligible for funding through Medicaid. By enabling psychiatric hospitals
to access this funding, the Murphy Bill could usher in an unprecedented era of re-institutionalization, going against the recommendations of the Supreme Court’s Olmstead decision,
which asserted in 1999 that people with mental health issues have the right to be in the least restrictive setting possible. If passed, the Murphy Bill will lead to large-scale re-institutionalization in hospitals for longer periods of time for people
who now generally have the right to live in supportive communities of their choosing.
The Murphy Bill threatens the recovery and community integration practices that current consumers of mental health services and survivors of coercive psychiatric interventions have worked so hard for over the last 40-plus years to create for those most
in need. In particular, the bill would dismantle the federal Substance Abuse and Mental Health Administration (SAMHSA), which actively funds and supports important efforts to rebuild the community
and family life of people dealing with mental health issues through non-medicalized institutions such as peer-run respites (short-term crisis centers managed by people living with mental health concerns and available to “self-referred” individuals seeking
to avoid hospitalization through support from peers). SAMHSA also supports suicide prevention initiatives, trauma-informed practices, Emotional CPR (an educational program aimed
at teaching people how to assist others through an emotional crisis), Wellness Recovery Action Planning and much more, all of which would suffer if SAMHSA were dismantled. The
bill would also threaten people’s rights by weakening state “Protection and Advocacy for People with Mental Illness” organizations, which
offer rights protections, and the Health Insurance Portability and Accountability Act, making it easier to force people into treatment.
Murphy and his supporters criticize opponents of the bill for being “against families.” They fail to acknowledge that families are not united in support of this bill. While the national headquarters of the National Alliance on Mental Illness (NAMI) has
come out in support of the bill, many local NAMI affiliates are against it. Activists who identify as current consumers of mental health services or survivors of psychiatric interventions are frequently approached by desperate family members who are
looking for alternatives to coercive and institutional responses to mental health crises. We are finding ways to include families because rebuilding strong family connections can be essential to recovery.
Community-Based Solutions to Mental Health Crises
Rosey Padgett in Prescott, Arizona, recently contacted the National Coalition for Mental Health Recovery because her son Nick was trapped in the mental health system. Currently, he is in the Arizona
State Hospital.
“Nick has been placed in mental hospitals approximately 30 different times over the past seven years,” Padgett says. “He has been court ordered and placed in many different group homes. All of the group homes have made his behavior worse due to being
forced into these situations when these homes are not an environment for healing. No wonder so many people with emotional and mental distress commit suicide: They feel dead inside and hopeless from being forced to take medications that make them feel
horrible.”
What has worked for Nick is connecting with other peers and having tremendous family support. A woman from the local Hearing Voices Network has begun visiting with him and providing peer support, as they are both voice hearers. He is doing so much better
that the doctors at Arizona State Hospital are talking about releasing him in a few months.
Nick’s story is similar to the stories of others around the country who are languishing in and out of hospitals. Often it is not what is happening in those hospitals that helps people reestablish a life; it is the family and community support they have
once they leave the hospital.
Murphy Bill proponents point to a lack of institutionally or medically directed mental health treatment as being a primary cause of the alarming rise of violent acts such as school shootings and suicide. However, when we look at this argument closely,
it falls apart.
This argument overlooks the fact that the link between mental health conditions and violence is minuscule, as many studies have shown. Mentalhealth.gov, a website run by the federal government, says:
The vast majority of people with mental health problems are no more likely to be violent than anyone else. Most people with mental illness are not violent and only 3 to 5 percent
of violent acts can be attributed to individuals living with a serious mental illness. In fact, people with severe mental illnesses are over 10 times more likely to be victims of violent crime than the general population…. When economist Richard Florida took a look at gun deaths and other social indicators, he found that higher populations, more stress, more immigrants and more mental illness didn’t correlate with more gun deaths. But he did find one telling correlation:
States with tighter gun control laws have fewer gun-related deaths.
We should probably be doing more questioning of the treatments themselves. For example, many antidepressant medications, such as Paxil, that are commonly prescribed to young people, have a black box warning that
they can increase suicidality among teenagers.
We all want to see violence and suicide go away, but passing legislation that imposes increased mental health screenings and forced treatments (including psychiatric medication) on unwilling individuals is neither an ethical nor an effective way to accomplish
this, especially given the risk of medications backfiring.
Standing Up for Peer-Run Recovery
Perhaps Murphy and supporters of his bill should ask those of us who have lived through extreme emotional distress for ideas and possible solutions. Thus far, the many activists who share the concerns I have outlined here have been denied a seat at the
table in congressional discussions of the Murphy bill, despite the recommendation made in 2003 by the President’s New Freedom Commission on Mental Health, which said that transformations of the mental health system should be led and informed by consumers
of mental health services.
What would survivors of extreme emotional distress say if we were at the table with Congressman Murphy?
Many of us would say that our mental health crises occur when we feel alone, abused and generally isolated from the rest of the world. We would thus raise our concern that, rather than reestablishing social connections, the current mental health system
often disconnects us even more and leads us to a lifelong dependence on the system itself.
Let’s take Dan, who as an adolescent contemplated shooting up his middle school. It wasn’t medication or therapy that prevented this terrible potential tragedy; Dan says it was talking to his friends at school and playing Dungeons and Dragons that grounded
him and gave him hope. In other words, peer support.
What would have happened if Dan had been flagged as a result of a mental health screening? He likely would have been removed from his social circles and placed in an institution, perhaps becoming permanently dependent on the system.
Dan is now a part of a peer-run recovery community called the Western Massachusetts Recovery Learning Community. He has his own place to live, a job, friends and a life, and is starring in the documentary HEALING VOICES.
The Recovery Learning Community helps people to establish much-needed social connections and gain a sense of belonging. This community is there when Dan needs it, and he doesn’t need a diagnosis or a referral to attend the many support groups and wellness
activities: the strength of places like the Recovery Learning Community is that they an integrated and open part of the broader community and not separate from it.
But if the Murphy Bill passes, places like this might cease to exist. By requiring expensive clinical oversight and unprecedented congressional control over federal grants, the Murphy Bill targets consumer-run organizations and peer specialists, making
it likely that national consumer-run organizations will be shut down, severely restricting what peer specialists can do and posing a threat to local peer-run organizations such as the Recovery Learning
Community.
Critics dismiss many opponents of the Murphy bill as being “anti-medication,” but in fact many of us take medications and have found them useful. Our philosophy is that people should have accurate information to make informed choices, including the choice
to use alternatives to medications. With the increase in violence and suicide and the alarming fact that people in the public mental health system die an average of 25 years younger than the rest of the population, shouldn’t researching and supporting
alternatives be a priority?
Current consumers of mental health services and survivors of psychiatric interventions are willing to share our knowledge and expertise.
Is anyone willing to listen?